Disclosure: Some of the mentioned attitudes and treatments in this article might offend or trigger you. Please note that the aim of this article is merely to try to explain the history of mental illness treatment and how things have evolved since. These methods do not reflect NISAD’s views in any way. Continue reading with caution.
To the modern mind, many of the past medical treatments for mental illness may seem cruel, barbaric and primitive or sometimes even dangerous.
Until fairly recently in time, very little was understood about how the human mind works.
I shall begin this article by taking you on a journey back in time to when illness was globally thought to be caused by evil spirits, punishment for trespassing or bad luck and the treatments would often do more harm than good.
The mental health history that follows below is predominantly from a Western perspective.
The Stone Age (approx 7000 BCE)
The understanding of mental treatment was hugely supernatural in the ancient periods, where mental illness, or any illness for that matter, was seen as the work of evil spirits, vengeful gods or sorcery.
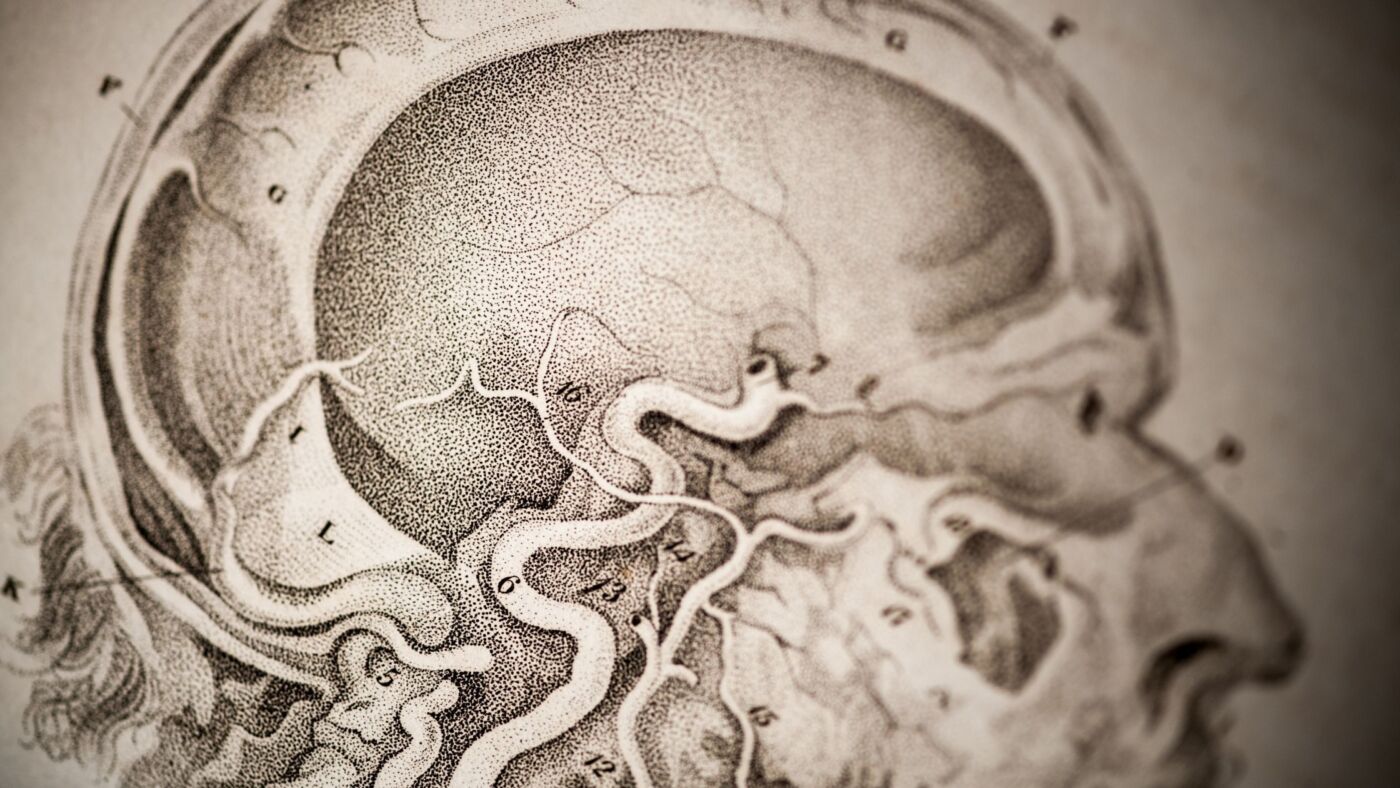
Thus the methods for treating mental illnesses were downright brutal and often resolved to drilling a big hole through the skull in order to release the evil spirits, a procedure known as trepanation.
This procedure was also used for non-psychological issues such as epilepsy and headaches. The small pieces of the skull cut out would usually be worn as a lucky charm to keep evil spirits away.
This was a very common procedure that dates back as far as 7000 years ago and was practised in places as diverse as Ancient Greece, France, Portugal, North and South America, Africa, Polynesia and the Far East including Russia.
Out of all skulls found in ancient burial sites across the world, 5-10% of them had trepanation holes in them (Livescience, 2018).
“Trepanation had been abandoned by most cultures by the end of the Middle Ages, but the practice was still being carried out in a few isolated parts of Africa and Polynesia until the early 1900s.” (BBC Earth, 2016)
Hippocrates’ influence
Hippocrates, also known as the father of medicine, was a firm believer in trepanation and wrote a guide on how to perform them. But the Greek period is more known for its revolutionary new idea that mental illness wasn’t the result of evil spirits or vengeful gods or other spiritual explanations. Thus new concepts were invented.
Hippocrates had ideas about how hysteria in women could be caused by a wandering womb (Wired, 2014).
The word hysteria derived from the Greek for “womb” and what the ancient Greeks or Romans or Arabs would consider to be hysteria was in fact a wide range of psychological disorders, from schizophrenia to panic attacks, which of course would happen to men as well as women. But the womb was to blame as it was believed to be able to wander around freely in the body all the way up to the throat, causing feelings of suffocation in the woman along with other physical as well as mental illness.
The womb was believed to have one weakness – scents. Pleasant smells near the vagina would lure the womb back in place. Foul smells for the woman to sniff would also make the womb wander back into place.
Pregnancy was prescribed in order to keep the bored, wandering womb in place. Running or other forms of exercise were close to forbidden as the womb was thought to be able to fall out from such activities.
Although this theory changed over time, there was still a lot of emphasis on wombs until Sigmund Freud made it abundantly clear that psychological disorders come from the brain, not from a malfunctioning womb (Wired, 2014).
“By the 19th century, physicians no longer believed that the womb wandered. But many of the ideas underlying the concept of hysteria — for instance, that female reproductive organs could be blamed for psychiatric problems — stuck around. In fact, as late as 1900, many asylums still performed routine gynecological examinations on their patients…”
(Livescience, 2019).
The theory of the four humors
The most commonly performed treatment in history, though, is bloodletting (History.com, 2018).
The medical practice of bloodletting also stems from Hippocrates, who believed illness stemmed from imbalanced humors in the body. Humors are bodily fluids such as blood, phlegm, yellow bile and black bile. Blood was later thought to be the dominant of these four humors and the balance would be restored by removing excess blood.
At that time surgeons thought that blood was created and used rather than circulating around the body. This led to thinking blood could stagnate in the body and cause mental and physical illness unless removed.
This practice was in most cases harmful rather than beneficial as there was a high risk of infection and catching diseases; especially if the procedure was done by putting the recommended fifty leeches on your body.
The leeches would be shared among patients, thus it made the risk of infections very high. Patients would also be given laxatives and emetics (to make them vomit) to restore the other humors (History.com, 2018).
Opposers
Now you might be thinking all ancient treatments of mental illness were primitive and pain-inflicting in different ways, but as a matter of fact, the people of the Roman province briefly had kinder options to choose from.
For example, there was Asclepiades of Bithynia (124 BCE – c. 30 BCE) who established a more humane approach to mental illness. Asclepiades believed that mental illness should be treated with harmony restoring activities such as fresh air, baths, exercise, music, massage and occupational therapy. He even prescribed for the patients to have conversations with well-established philosophers over a glass of wine (Encyclopædia Britannica, 2011).
Unfortunately, Asclepiades’ work did not survive and was only rediscovered through the mostly hostile accounts of later authors and physicians and his work is seen as a philosophical detective story (King, Helen., J. T. Vallance, 1992).
Unsurprisingly the success rate of Asclepiades’ work was very high; until Claudius Galen (Encyclopædia Britannica, 2020) began to practise medicine in Rome in CE 164.
Although Galen rejected the previous theory of the wandering womb, he returned to Hippocrates theory of the humors and declared blood to be the most important humor, which made this theory become standard practice again for many many years to come.
The practice of bloodletting continued sporadically in the West until around the 1940s, but mostly for treating physical illness such as pneumonia.
Middle Ages – 500 CE – 1500
The most widely believed philosophy during the middle ages was that the soul governs the body. This belief was influenced heavily by the religious influence of the churches and led to the scientific beliefs that demons were the cause of mental illness. Treatments included exorcisms, hearing mass and drinking a cold glass of water.
All of these methods were intended to make the demon so uncomfortable it would leave the body and thus cure the illness.
Women especially would be accused of practising witchcraft, which is another story on its own. The church would often make amulets for the people living with mental illness in order to protect and soothe troubled minds (Foerschner, A. M., 2010).

Until this era, the responsibility to care for the patient living with mental illness would lie upon the family.
Regrettably, there was a lot of stigma around having a family member with mental illness. It could even be seen as a blight on the family honour as it was interpreted as suggested defects in the family bloodline.
This tragically led to people with mental illness being heavily subdued to being imprisoned for life by their own family members who didn’t know how to deal with (rather than help) the person living with mental illness.
Beatings as punishment for antisocial behaviour was common. Others were checked into general hospitals, but they were often abandoned and ignored.
“Family having custody of mentally ill patients was for a long time seen as a source of shame and humiliation; many families resorted to hiding their loved ones in cellars, sometimes caging them, delegating them to servants’ care, or simply abandoning them, leaving their mentally unhealthy flesh and blood on the streets as beggars” (Sunrisehouse, 2020)
With the heavy influence of religion, there was luckily a less callous option to being left to fend for yourself or being locked away. A public institution of so-called Workhouses was set up to give people living with mental illness a roof over their heads.
Although the overall message was to pray and ask for forgiveness, which had very little success, giving the people a purpose and a roof over their heads turned out to be very positive. But it didn’t take long until the workhouses were overflowing and unfortunately the treatment of the people living with mental illness took a turn for the worse.
Asylums
Asylums were more commonly known as ‘madhouses’ with the offensive word ‘mad’ as a broad term for people living with mental illnesses (the term I have aimed to use in this article).
The asylums became widely used in the 15th century and served as penal institutions where people living with mental illness could be abandoned and hidden away from society, often in very poor conditions, which was the main purpose rather than helping the patients cope with their mental illnesses. Treatment as such was completely out of the question.
At the beginning of the 15th century, all of society’s ‘undesirables’ such as thieves, the homeless, the unemployed and people living with mental illness were all locked away in the asylums – most of them institutionalized against their will, chained up in dark, filthy cells and even exhibited, for a fee, to wealthy people for their entertainment.
The people living with mental illness, in particular, were seen and treated like animals who did not have the capacity to reason, could not control themselves, were capable of violence without provocation, did not have the same physical sensitivity to pain or temperature, and could live in miserable conditions without complaint (Farreras, I. G., 2020).
Although one can’t say with complete certainty that the following is what happened, there are still several reports that state that the cells were never cleaned and visitors only came to bring food for the patients.
The patients were thus forced to live in complete solitude surrounded by their own filth that no one came to clean up, with only a layer of straw as a comfort from the hard, cold floor. The iron cuffs and collars permitted just enough movement for the patients to feed themselves but made it impossible to lie down for sleeping so the patients were forced to sleep sitting upright. No attempts were made to inspect that these facilities or the food were up to standard, not to mention how their treatments would help the patients feel better (Foerschner, A. M., 2010).
Industrial revolution – 1760 CE – 1830 CE
Only families of means would be able to afford to have doctors sent to their house to give the family instructions on how to care for the family member living with mental illness.
Unfortunately, most physicians still didn’t know how to care for people living with mental illness and the same methods ie the theory of the bodily humors (purging, leeches etc.), would be used over and over with very little sign of improvement.
When the family couldn’t support them anymore the person living with mental illness could be sent to a private home instead of an institution such as an asylum.
For poorer families, there really were only two options in regard to caring for the family member living with mental illness – asylums or the streets.
Asylums had luckily started to become somewhat more humane places, thanks to how protests rose over the unsanitary and callous conditions their patients were held under for so many years.
During the industrial revolution, shackles were removed all across Europe and the patients would be seen more like guests rather than prisoners. Keeping good hygiene and keeping the patients in well-lit, airy rooms were recommended thanks to the humanitarian reforms all across Europe, starting in France 1792 and then spreading across Europe and the US (Farreras, I. G., 2020).
This moral treatment was highly successful and it was the first time since Asclepiades of Bithynia’s time, that anyone had thought to rehabilitate, rather than hide away, the patients. Patients would similarly be encouraged to take part in manual labour and intellectual conversations and were expected to act politely and in a civilized manner in this new home-like environment (Sunrisehouse, 2020).
During this time there was still quite a lot of controversy on whether mental illness was the result of somatogenic (arising from physiological causes) or psychogenic (arising from emotional or mental stressors, or from psychological or psychiatric disorders) reasons.
It was particularly difficult to understand the concept of hysteria, which although a mental condition, could lead to physical symptoms such as blindness or paralysis, without any apparent explanation, which is where the important work of James Braid makes an entrance.
Victorian Era – 1837-1901
In the 19th century, hypnosis was more commonly known as mesmerism (Britannica, 2020), until the British surgeon James Braid coined the term hypnosis in 1843. Braid described the state of hypnosis as a nervous kind of sleep induced by fatigue from staring intensely at a bright inanimate object.
Braid meant that hypnosis was a therapeutic possibility in alleviating mental illness of a “nervous” disposition, such as anxiety, before surgeries. Although Braid focused more on physical illness, his findings made a massive imprint on how people viewed mental illness by proposing a psychogenic treatment for the removal of symptoms (Britannica, 2020).
Braid’s work laid the ground for physician Josef Breuer (1842–1925) and neurologist Sigmund Freud (1856–1939) who would later adopt this psychogenic explanation for mental illness by treating hysteria through hypnosis, which eventually led to the cathartic method that became the precursor for psychoanalysis during the first half of the 20th century (Farreras, I. G., 2020).
But going back to the 19th century, the Victorian era was particularly difficult for Western women, who were then seen as men’s property. Although 1st wave feminism (approx. 1848-1920) was growing rapidly, the men they were married to would often respond by putting women who disobeyed in these so-called insane asylums.
Refusal of traditional gender rules could thus be seen as an abnormality that would legitimise sending them to the asylums. Psychiatrists were often hired by husbands and fathers to probe their wives’ and daughters’ “abnormal” behaviours. In some states in America, no proof of said insanity was needed which made it very easy to get women locked up for life in order to attain the male dominance status quo (The Atlantic, 2017).
“The reasons men cited for such inquisitions were manifold. It could have been anything from exhaustion, overeducation, or premenstrual syndrome to being unmarried or indulging unconventional sexual impulses (such as masturbation). On the most basic level, it was never about mental acuity or medical treatment; it was about exerting control over women’s lives and bodies—all under the guise of medicine” (The Atlantic, 2017).
Towards the end of the 19th century, the previous moral treatment method died out towards the end of the Victorian era. Critics claimed it made the patients “too cosy” and dependent on their doctors and asylum staff for comfort. Make no mistake that even the moral treatment included immoral treatments and sanctions, however, these made a big return as the moral treatment method died out. Patients would be physically restrained with leather wristlets and straitjackets, sometimes for hours and hours, as well as being subjected to ice baths, referred to then as Hydrotherapy (Talkspace, 2017).
“Warm, or more commonly, cold water, allegedly reduced agitation, particularly for those experiencing manic episodes. People were either submerged in a bath for hours at a time, mummified in a wrapped ‘pack’, or sprayed with a deluge of shockingly cold water in showers” (Talkspace, 2017).
20th century
During the first half of the 20th century, the understanding and treatment of mental illness took a big step in the right direction with the founding of psychoanalysis by Sigmund Freud, an Austrian neurologist and psychiatrist.
Between the years of 1888 and 1939, Sigmund Freud published twenty-four volumes explaining his thoughts about personality and psychopathology. Patients were asked to write journals and dream analysis talk therapy gained popularity. Freud’s methods, although widely trained today, met heavy criticism and fell out of favour around the mid-50s (Foerschner, A. M., 2010).
Overall one could describe the beginning of the 20th century as a bit more “hands-on” in regards to treating mental illnesses. Whereas before patients would still be treated with the theory of the humors ie. purging, bloodletting etc., new discoveries were made and added to the shortlist of treatments.
The 1930s brought with them four different somatotherapies, meaning the treatment of mental illness by physical means rather than psychotherapy. Some of these treatments were well-researched and successful whereas some treatments were not, which led to the belief that asylum staff used these methods to keep the patients more manageable, rather than to help them improve.
ICT – Insulin shock therapy
In 1927 the treatment of insulin shock therapy was introduced as a way of treating Schizophrenia.
A doctor or other trained staff would inject high doses of insulin six days a week for up to two months, although periods as long as 2 years have been documented, as different asylums would have their own standard guidelines.
Back then it was believed that large fluctuations in insulin levels could alter the function of the brain.
The comas would last 1-4 hours each. The mortality rate varied between 1 and 10 percent and would often cause other health issues such as morbid obesity as well as amnesia and had no effect whatsoever in regards to treating mental illness.
The method was used until the 1960s in Europe and the US. It was used in China and the Soviet Union until the 1970s (CSP Online, 2016).
Metrazol convulsive therapy/ECT
Electroconvulsive Therapy, formerly known as electroshock therapy was incidentally discovered in the late 1930s. The people working at the asylums around this time had a good understanding of mental illnesses and discovered that psychotic patients who also suffered from epilepsy, seemed to improve mentally after a seizure.
With this information in mind, the Portuguese psychiatrist Ladislas Meduna began experimenting with different ways to induce seizures in patients. One of the ways found was to slightly overdose patients with the stimulant drug Metrazol ie Metrazol convulsive therapy.
After the patients’ induced seizures, the psychotic symptoms successfully diminished, although it was later discovered that Metrazol produced violent thrashing convulsions which would commonly result in vertebral fractures in 20-30% of the patients.
Additionally, the patients would feel morbidly apprehensive before the convulsions began. A new way to induce seizures needed to be found (Psychology Today, 2018).
Incidentally, around the same time, Italian neurologist Ugo Cerletti was experimenting with seizure induction in dogs by delivering electrical shocks directly to their heads. He had got the idea from watching a butcher who had done this procedure to pigs, in order to put these in a coma-like state, right before slaughtering them.
This led Cerletti to wonder whether doing this to humans would similarly produce anaesthesia before provoking convulsions. Thus electroconvulsive therapy was born and Cerletti developed the first ECT device that he tested on a patient with schizophrenia.
Afterwards, the patient’s condition improved markedly. This was the first major breakthrough in biological psychiatry and won Cerletti the Nobel Prize in medicine in the 1930s (Psychology Today, 2018).
Although the method of electroconvulsive therapy seemed promising, its widespread involuntary use was found to cause patients distress and terror.
ECT was also used as a threat for uncooperative patients in asylums. The use of ECT fell out of favour in the 1960s and 1970s but gradually reemerged for use on patients who did not respond to medication.
The (largely abandoned) use of involuntary ECT continues to be a controversial treatment in psychiatry and this varies from country to country, depending on local mental health laws. ECT now tends to be used as a last resort for mental illnesses that cannot be treated by standard methods, such as severe depression with symptoms of psychosis. (Sunrise House, 2020)
Lobotomy
A lobotomy is a neurosurgical operation that involves severing connections in the brain’s prefrontal lobe. Although the side effects were many and sometimes severe, lobotomies were widely performed for over two decades.
Discovered by The Portuguese neurologist António Egas Moniz (Livescience, 2014) in 1935, he earned a Nobel prize for his discovery.
There were a range of different ways to perform the lobotomy, but the most common one was made with an instrument that looks very similar to an ice pick, which was inserted through the eye socket of the patient and then hammered into the brain with a hammer and then wriggled around in order to separate the frontal lobes from the rest of the brain.
It was neither an elegant nor comfortable procedure (performed without anaesthesia) and could be performed by any physician. Multiple lobotomies could be done in a day, without the need for either a traditional surgeon or an operating room. As such it was considered a miracle quick fix to cure a wide range of mental illnesses such as anxiety, depression, compulsory disorders, bipolar disorder, schizophrenia and so on (Wired, 2011).
Lobotomies could be seen as a way to take away the responsibility from society, and the patients’ family would be left to pick up the pieces. Around 5% died from the lobotomies and some died by suicide afterwards (Valenstein, E.A., 1997).
The ones who survived lost much of their independence not to mention their personality. Other common side effects included apathy, bladder and bowel incontinence, catatonia, mutism, seizures and even permanent paralysis.
The biggest problem was that none of the lobotomies were properly followed up later; a patient could walk out the door and be out of sight, out of mind. What’s important to understand about lobotomies is that during that time there were still no good ways to treat mental illnesses and sometimes the alternatives were much worse.
“When I visited mental hospitals… you saw straitjackets, padded cells, and it was patently apparent that some of the patients were, I’m sorry to say, subjected to physical violence,” recalls retired neurosurgeon Jason Brice (BBC News, 8 November 2011).
Nowadays lobotomies are never performed as a treatment for mental illness.
Introduction to medicines
In the 1950s the lobotomies as a standard practice stopped as the much more effective, and far less drastic alternative, antidepressant and antipsychotic medication was discovered through research.
These medicines meant a change of attitude towards people living with mental illness.
Whereas before, all of the methods mentioned above would be used on different people with different illnesses, mostly to sedate them in one way or another, specific medicines would be made to treat specific illnesses.
Asylums in most parts of the world eventually got abandoned or found other purposes such as becoming research centres for mental illnesses, which says a lot about how the general attitude towards mental illnesses changed for the better. The closing of the asylums, however, didn’t happen overnight and happened in different places around different parts of the world. It is to a degree still an ongoing process. China for example still has their Ankang Asylums running, where people living with mental illnesses are sadly still subjected to violence and restraints. There are sadly a lot of reports about discrimination towards people living with mental illness in China (Bitter Winter, 2019).
Conclusion
You may have found that this article was uncomfortable to read. Although interesting to analyze, the subject of how people living with mental illness have been treated throughout time is likely to leave a sour taste in most people’s mouths.
It makes you wonder how then considered great minds like Hippocrates and Galen were let to ravage freely with people’s minds and bodies. It might be a small consolation, but still, we have, overall, come a long way since the stone age in regards to treating and understanding mental illness.
Modern treatments rely more on support and counselling combined with specific medications and follow-ups. Sometimes alternative medicine and mindful exercises are encouraged.
Although the system isn’t perfect I think it’s safe to say that it’s heading in the right direction. If anything you have read in this article has concerned you or if you think we’ve missed anything that would be interesting to include, please get in touch with us at NISAD.
Definitions:
BCE – Before Common Era
CE – Common Era
Why the term “living with mental illness” has been used: Healthpartners’ definition
References:
Bradford, Alina. (2018), ‘What Is Trepanation?’, Livescience, May 17, Access date: 9 September 2020, from
https://www.livescience.com/62591-trepanation-explained.html
Wylie, Robin. (2016), ‘Why our ancestors drilled holes into each other’s skulls’, BBC Earth, 29 August, Access date: 31 August 2020, from
http://www.bbc.com/earth/story/20160826-why-our-ancestors-drilled-holes-in-each-others-skulls
Simon, Matt. (2014), ‘Fantastically Wrong: The Theory of the Wandering Wombs That Drove Women to Madness’, Wired, 5 June, Access date: 27 August 2020, from
https://www.wired.com/2014/05/fantastically-wrong-wandering-womb/
Whitcomb, Isobel. (2019), ‘7 Sexist Ideas That Once Plagued Science’, Livescience, 30 September, Access date: 26 October 2020, from
https://www.livescience.com/sexist-medical-ideas-about-women.html
Cohen, Jennie. (2018), ‘A brief history of bloodletting’, History.com, 29 August, Access date: 27 October 2020, from
https://www.history.com/news/a-brief-history-of-bloodletting
The Editors of Encyclopaedia Britannica. (2011), ‘Asclepiades Of Bithynia’, Encyclopædia Britannica, 26 September, Access date: 10 September 2020, from
https://www.britannica.com/biography/Asclepiades-of-Bithynia
King, H. (1992). J. T. Vallance: The Lost Theory of Asclepiades of Bithynia. Pp. xi 162. Oxford: Clarendon Press, 1990. The Classical Review, 42(1), 231-232.
Nutton, Vivian. (2020), ‘Galen’, Encyclopædia Britannica, 1 January, Access date: 25 August 2020, from
https://www.britannica.com/biography/Galen
Foerschner, A. M. (2010). ‘The History of Mental Illness: From Skull Drills to Happy Pills’ Inquiries Journal/Student Pulse, 2(09). Access date 29 October, from http://www.inquiriesjournal.com/articles/1673/2/the-history-of-mental-illness-from-skull-drills-to-happy-pills
Editorial Staff (2020). ‘The History & Evolution of Mental Health & Treatment’, Sunrise House, 5 August, Access date: 3 November 2020, from
https://sunrisehouse.com/research/history-evolution-mental-health-treatment/
Farreras, I. G. (2020). History of mental illness. In R. Biswas-Diener & E. Diener (Eds), Noba textbook series: Psychology. Champaign, IL: DEF publishers. Acces date 30 October, from
http://noba.to/65w3s7ex
The Editors of Encyclopaedia Britannica. (2020), ‘James Braid’, Encyclopædia Britannica, March 21, Acces date: 2 November 2020, from
https://www.britannica.com/biography/James-Braid-British-surgeon
Blazevich, Jenna. (2017), ‘How Victorian Women Were Oppressed Through the Use of Psychiatry’, The Atlantic, November 3, Acces date: 29 October 2020, from
https://www.theatlantic.com/sponsored/netflix-2017/how-victorian-women-were-oppressed-through-the-use-of-psychiatry/1607/
Concordia University, St Paul. (2016), ‘A HISTORY OF MENTAL ILLNESS TREATMENT: OBSOLETE PRACTICES’, CSPonline, 14 October, Access date: 3 November 2020, from
https://online.csp.edu/blog/psychology/history-of-mental-illness-treatment/
Mark L. Ruffalo, (2018), ‘A Brief History of Electroconvulsive Therapy – The story of a misunderstood but effective treatment’, Psychology Today, 3 November, Access date: 2 November 2020, from
https://www.psychologytoday.com/gb/blog/freud-fluoxetine/201811/brief-history-electroconvulsive-therapy
Lewis, Tanya. (2014), ‘Lobotomy: Definition, Procedure & History’, Livescience, 29 August, Access date: 26 August 2020, from
https://www.livescience.com/42199-lobotomy-definition.html
Newitz, Annalee. (2011), ‘The Strange Past and Promising Future of the Lobotomy’, Wired, 31 March, Access date: 31 August 2020, from
https://www.wired.com/2011/03/lobotomy-history/
Valenstein, Elliot A., History of Psychosurgery. In: Greenblatt, Samuel H. (ed.). A History of Neurosurgery: In Its Scientific and Professional Contexts. Contributing editors Dagi, T. Forcht; Epstein, Mel H.. Park Ridge, IL: The American Association of Neurological Surgeons; 1997. ISBN 978-1-879284-17-3. p. 499–516.
Levinson, Hugh. (2011), ‘The strange and curious history of lobotomy’, BBC News, 8 November, Access date: 13 August 2020, from https://www.bbc.co.uk/news/magazine-15629160
Zhang, Wenshu. (2019), ‘Dissidents, Believers Jailed in Psychiatric Hospitals’, Bitter Winter, 5 December, Access date: 11 November 2020, from
https://bitterwinter.org/dissidents-believers-jailed-in-psychiatric-hospitals/

Findus Krantz
Social psychologist and analyst
Findus is a social psychologist and analyst working with NISAD on a number of our projects – in particular, currently, with the development of ELK-Health’s #CertainAbout Uncertainty programme.
If you would like to be one of the first to use this programme, please contact us. The programme is completely free and designed to support people who feel that things, currently, are causing them stress, anxiety or depression.